Introduction
An intrauterine device (IUD) is a small, T-shaped contraceptive device that is inserted into the uterus in order to prevent pregnancy. IUDs are one of the most effective forms of birth control available, with a failure rate of less than 1%. It’s estimated that more than 200 million women around the world use IUDs for contraception.
In this article, we’ll take a closer look at how IUDs work, from the science behind their mechanism of action to the different types available, the pros and cons of using them, and the steps involved in inserting and removing them.
Exploring the Science Behind IUDs: How Do They Function?
To understand how IUDs work, it’s important to first understand the anatomy and physiology of the uterus. The uterus is a hollow, pear-shaped organ made up of muscle and connective tissue. It’s lined with a thin layer of cells called the endometrium. During ovulation, an egg is released from the ovaries and travels through the fallopian tubes to the uterus. If the egg is fertilized by sperm, it will implant itself in the endometrium, where it can grow and develop. If the egg is not fertilized, the endometrium will shed, resulting in menstrual bleeding.
The mechanism of action of IUDs is twofold. First, they release either copper or hormones, which act as a barrier to block sperm from entering the uterus and fertilizing an egg. Second, they create a hostile environment within the uterus that prevents a fertilized egg from implanting in the endometrium.

Different Types of IUDs and How They Function
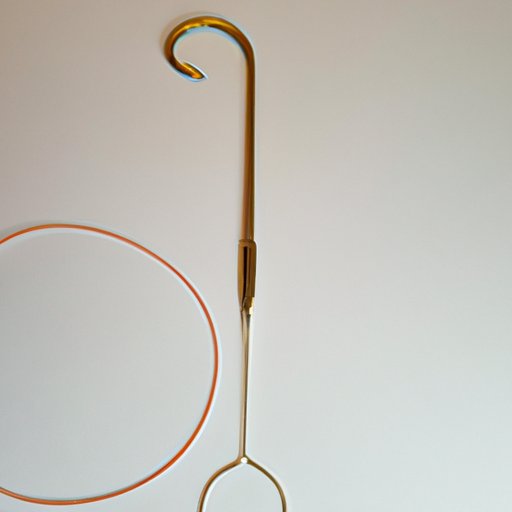
There are two main types of IUDs: copper and hormonal. Copper IUDs are non-hormonal devices that contain copper wire coiled around the stem of the T-shaped device. The copper ions released by the IUD interfere with the movement of sperm, preventing it from fertilizing an egg. Hormonal IUDs, on the other hand, release a synthetic version of the hormone progestin, which thickens the cervical mucus to block sperm from reaching the uterus and thins the lining of the uterus to prevent a fertilized egg from implanting.

Pros and Cons of IUDs
Like any form of contraception, IUDs come with both benefits and risks. On the plus side, IUDs are one of the most effective forms of birth control available, with a failure rate of less than 1%. They’re also long-acting and reversible, meaning they can be removed at any time if you decide you want to become pregnant. IUDs are also relatively low maintenance; once it’s inserted, you don’t have to think about it again until it needs to be replaced.
On the downside, IUDs can cause side effects such as cramping and spotting between periods. They also don’t protect against sexually transmitted diseases (STDs). Additionally, there is a risk of expulsion (when the IUD falls out of the uterus) or perforation (when the IUD punctures the wall of the uterus). This is rare, but it can occur, so it’s important to talk to your doctor about the potential risks before deciding whether or not an IUD is right for you.
Steps Involved in Inserting and Removing an IUD
Inserting and removing an IUD requires a short office visit. During the procedure, the doctor will use a speculum to open the vagina, then use forceps to insert the IUD into the uterus. The process usually takes less than 10 minutes and can be done without anesthesia. After the IUD is inserted, the strings attached to it will hang down into the vagina, allowing you to check that the IUD is still in place.
Removing an IUD is just as easy as inserting it. The doctor will use forceps to grasp the strings and gently pull the IUD out of the uterus. Again, the whole process usually takes less than 10 minutes and can be done without anesthesia.
Conclusion
IUDs are a safe, effective, and long-lasting form of contraception. They come in two main varieties—copper and hormonal—and each works in slightly different ways. While IUDs come with some risks, these risks are rare and can be minimized with regular follow-up visits and careful monitoring. If you’re considering an IUD as a form of birth control, it’s important to talk to your doctor about the potential risks and benefits.
For more information about IUDs, visit Planned Parenthood, American College of Obstetricians and Gynecologists, or Family Planning Association.
(Note: Is this article not meeting your expectations? Do you have knowledge or insights to share? Unlock new opportunities and expand your reach by joining our authors team. Click Registration to join us and share your expertise with our readers.)